Closing the Loop by Operationalizing Systems Engineering and Design (CLOSED)
Motivation:
Specific Aims :
Aim 1:Use systems engineering and patient engagement to design, develop, and refine a highly reliable “closed loop” system for diagnostic tests and referrals that ensures diagnostic orders and follow-up occur reliably within clinically- and patient-important time-frames.
Aim 2: Use systems engineering and patient engagement to design, develop, and refine a highly reliable “closed loop” system for symptoms that ensures clinicians receive and act on feedback about evolving symptoms and physical findings of concern to patients or clinicians.
Aim 3: Design for generalizability across health systems more broadly so that the processes created in Aims 1 and 2 are effective in (1) a practice in an underserved community, (2) a large tele-medicine system, and (3) a representative range of simulated other health system settings and populations.
Partners:
Sunday, June 2, 2019
Sunday, June 2, 2019
Approach:
Sunday, June 2, 2019
Results to Date:
Epidemic Surge Model Use to Improve Patient, Staff, and System Safety and Resiliency
James C. Benneyan, PhD (PI), Healthcare Systems Engineering Institute, Northeastern University, Boston MA
Agency for Healthcare Research and Quality (grant #: R01 HS28458-01A1)
For more information: Press Release
Background
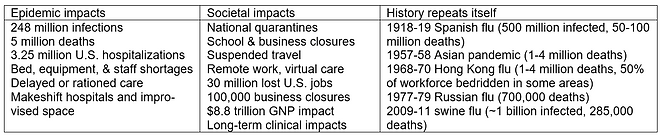
The HSyE Institute has received a five-year $2 million R01 research grant from the Agency for Healthcare Research and Quality to develop better epidemic surge, hospital capacity, and decision-support modeling approaches. As tragically evidenced by COVID-19, epidemics can surge dramatically, change continually, and significantly strain health systems, for example with SARS-CoV-2 in its first two years infecting over 250 million worldwide, killing over 5 million, and impacting safe equitable care, including makeshift rooming, equipment and staff shortages, rationed care, and other crisis management.
Broad agreement also exists that future epidemics will occur, better preparedness is needed for managing surges, and much should be learned from the COVID-19 pandemic. Among other needs, better real-time methods are needed to anticipate hospital, equipment, and staff capacities and shortages to allow earlier preemptive mitigation. As with past epidemics, affected regions and states were unprepared to handle unpredictable and significantly differing local surges in timing, severity, duration, and recurrence, with broad agreement of the need to be better prepared for future epidemics, including how best to leverage facility-level operational models to safely manage care capacity surges.
Research Objectives
This project will refine, evaluate, and study the use, accuracy, and impact on patient, staff, and system safety of a novel facility-specific 30-day ahead rolling bed, equipment, and staff surge capacity model, evaluating performance under a wide range of past and future scenarios via both retrospective data from varied health partners and prospective computer simulation of future epidemics. Specific research objectives are to:
1. Conduct modeling research to further refine results to-date, optimize accuracy, and address identified technical needs,
2. Evaluate impacts and accuracy of the developed models on improved hospital capacity and safety under a wide range of simulated future and historical surge scenarios, and
3. Maximize future utility by studying how our models were used in practice during COVID-19, the model adoption process, types of resulting actions, barriers to use, and user perceptions of utility, accuracy, and model-based decision-making.
Anticipated results include validated robust models for preemptively responding to care surges, reduced unsafe hospital crisis management conditions during future epidemics, and improved understanding of how to best use systems engineering models to address epidemic surges and other important public health and care delivery problems.
.png)
_edited.jpg)
Research Team and Partners
-
Dr. James Benneyan (Principal Investigator), Professor of Industrial Engineering and Operations Research and Director of the Healthcare Systems Engineering Institute at Northeastern University.
-
Dr. Michael Rosenblatt (Co-Investigator), Chief Medical Officer at BILH’s Lahey Hospital and Medical Center
-
Laura Senier, PhD, MPH, Institute on Urban Health Research, Northeastern University.
-
National Advisory Committee with expertise in patient safety, hospital capacity, surge management, technology adoption, systems modeling, qualitative methods, intervention analysis, and human factors
Project Sites
-
Seven U.S. health systems comprising 74 hospitals) of varied in size, patient populations, and surge experiences
-
We are actively seeking additional participants
Results to Date
Our preliminary work has developed and integrated several models that accurately predict short-term regional surges, self-adapt on an ongoing basis to local changes in epidemic trajectories, and estimate 4-week ahead day-to-day unit-specific bed, staff, and equipment demand, availability, and shortages, allowing health systems to anticipate and pre-emptively adapt to local dynamics (i.e. system resiliency). Each model can be used separately or together and are based on differential equations, logistic growth curve fitting, statistical change detection methods, and computer simulation to account for inherent uncertainties and variability. In contrast to the several more macro-level epidemic models often in the media, ours produce more granular actionable details (e.g., daily patient census by type, admission units, lengths of stay, flow paths, and associated equipment, PPE, staffing needs) to help hospitals preemptively make real-time day-to-day space, staffing, and resources decisions. The combined model has been used by multiple health systems, 14-day ahead 85-95% accuracy.
.png)
.png)
“We have the opportunity to learn from innovations and challenges of the healthcare delivery system in order to accelerate recovery and prepare for future pandemics” (AHRQ Director Dr. David Meyers)
Publications
-
Benneyan J, Bargal B, Yap S, Kaya Y. A Hospital Surge Capacity Bed, Equipment, and Staff Demand Planning Model. Healthcare Systems Engineering Institute: Northeastern University; 2020. https://www.hsye.org/_files/ugd/8e76e9_9b72c3129a3b401388db22f1623a0913.pdf
-
Benneyan J, Rosenblatt M, Bargal B, Yap S, Kaya Y. Modeling Hospital-Specific Bed, PPE, and Staff Surge Capacity, working paper.
-
Duan X, Benneyan J (2022). Prospective Surveillance for Epidemic Outbreaks Using Updating Rolling Window Scan Statistics, under review with Statistics in Medicine.
-
Benneyan J, Nehls N, Ilieş I. Performance and corrections to a proposed statistical control chart method for monitoring Covid-19 infection and mortality data, under review with International Journal for Quality in Healthcare. 2020.
-
Benneyan J, Gehrke C, Ilieş, I, Nehls N (2021). Community and campus Covid-19 risks from university reopening scenarios: Model-based analysis, JMIR Public Health and Surveillance, 7(4):e24292, doi: 10.2196/24292
